Aitor Rius – Medical Devices (& In Vitro) Regulatory and Quality Consultant, Rephine
Beyond UDI assignment, there are more than a few new requirements in regard to traceability to successfully obtain the MDR and IVDR certificate, and not all of them are easy to understand. That is why manufacturers often have questions such as:
- What manufacturers need to know before identifying their MD or IVD?
- The UDI allows for a clear and unambiguous identification of specific devices on the market;
- provides access to useful information about devices;
- Makes traceability of devices more efficient;
- Allows easier recall of devices;
- Combats counterfeiting;
- Improves patient safety;
- It will be and addition, not a substitute for, the existing labelling requirements of medical devices.
To find out more about our services, or to discuss a specific requirement, get in touch with our Medical Devices expert.
UDI = UDI-DI (Device Identifier, specific to a model of MD and manufacturer) + UDI-PI (Product Identifier, specific to units of device production (serial nº, lot nº, software date, expiry/manufacturing date, etc.). UDI has to be placed on the label of the device, on the device itself or on its packaging.
Basic UDI-DI = identification number that is not for a specific product but for a group of products. Primary identifier of a device model. It groups devices by intended purpose, risk class and design & manufacturing characteristics. Code which is referenced in the certificates, technical dossier and EU Declaration of Conformity and must be provided to the UDI database. Not in trade item.
The UDIs are issued by issuing entities, designed by the European Commission, which are responsible to operate a system that generates UDI codes. Nevertheless, those issuing entities shall provide the manufacturers tools and guidelines to collect all the device information needed for their systems to generate the new UDI and Basic UDI-DIs.
- GS1 AISBL
- Health Industry Business Communications Council (HIBCC)
- International Council for Commonality in Blood Banking Automation (ICCBBA)
- Informationsstelle für Arzneispezialitäten (IFA) GmbH
Rephine can assist you to get in touch or fully manage your UDI application.
No, same UDI requirements and assignation methodology are implemented to every device, independently of the risk classification. However, the UDI implementation date is indeed influenced by the device risk or type of device:
Device as per Regulation (EU) 2017/745 (MDR) and 2017/746 (IVDR) | Implantable devices and Class III MD / Class D IVD | Class IIa and Class IIb MD / Class C and B IVD | Class I MD / Class A IVD |
Placing UDI-carriers on the labels of the devices – MDR Article 123(3)(f), Article 27(4) | 26 May 2021 | 26 May 2023 | 26 May 2025 |
Direct marking of the reusable devices – MDR Article 123(3)(g), Article 27(4) | 26 May 2023 | 26 May 2025 | 26 May 2027 |
IVDR Placing UDI-carriers on the labels of devices (IVDR Article 113(3)(e), Article 24(4)) | 26 May 2023 | 26 May 2025 | 26 May 2027 |
Any manufacturer has the regulatory requirement to assign a UDI and Basic UDI to their device(s), as per MDR and IVDR dictate. Both, UDI and Basic UDI-DI are needed to obtain the CE certificate.
Basic UDI-DI is an administration number which appears on:
- Certificates (Notified Bodies).
- Declaration of Conformity.
- Technical Documentation.
- Summary of Safety and Performance.
- Certificate of Free Sale.
- EUDAMED register.
Of note, Basic UDI-DI shall not be placed on the device, neither any packaging or labelling item.
On the other hand, the UDI shall appear on the device through the UDI-carrier on the device and to all higher levels of packaging: UDI has to be placed on the label of the device, on the device itself or on its packaging. The UDI-carrier would mean the format in which the UDI is seen:
- Automatic Identification and Data Capture (AIDC), is a technology used to automatically capture data. AIDC technologies include bar codes, smart cards, biometrics and RFID (Radio Frequency Identification).
- Human Readable Interpretation (HRI), a legible interpretation of data characters encoded in the UDI carrier. Would be relevant in case there is no automatic system to read the code.
Particular features apply to the specific portion of the UDI that comes from UDI-PI. Any lot number, serial number, software identification or expiry date that appears anywhere else on the label used to recognize the device production unit, shall be part of the UDI-PI. In general, the manufacturing date is not considered as a UDI-PI identifier, but in case the only production tracing item was the manufacturing date, yet this shall be used as the UDI-PI.
The UDI-PI characteristics such as the lot or serial number shall be provided by the manufacturer and introduced on the code assignment.
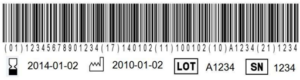
Figure 1. The different types of UDI-PIs include expiration date (17), manufacturing date (11), lot number (10) and/or serial number (21). (01) identifier corresponds to the UDI-DI part of the UDI code.
UDI requirements apply to all medical devices and in vitro diagnostics devices, except to custom-made and investigational devices. Specifically for software, only software that is commercially available on its own and software that constitutes a medical device in itself (i.e. Medical Device Software, MDSW) shall be subjected to these requirements.
As well as the rest of devices, the UDI-PIs (serial/lot number, manufacturing date or expiry date) together with the UDI-DI shall appear on the device labels and the device itself, which, in the case of MDSW, could be elements of the user interface.
In the same way, a Basic UDI-DI is also required for MDSW under the Medical Device Regulation (EU) 2017/745 (MDR). The Basic UDI-DI connects MDSW from the same manufacturer (same Single Registration Number, SRN) which have the same intended purpose, same risk class, and same essential design and manufacturing characteristics.
Therefore, the strategy needed to be followed to assign UDI codes to MDSW is the same that for the rest of devices:
- Register with an EU-accredited issuing entity for UDI assignment.
- Set up a UDI Management procedure ruled under QMS.
- Assign the individual UDI-DIs at the software system level, for MDSW that is commercially available on its own
- Assign the Basic UDI-DI.
- Build up the UDI-PIs. In this case, the software system identification would be considered the manufacturing traceability item, and shall be part of the UDI-PI.
- Register and upload UDI data in EUDAMED.
- Select an appropriate UDI carrier:
- For MDSW delivered on a physical medium (e.g. CD, USB key), each packaging level shall bear both the human-readable and machine-readable (i.e. AIDC) representation of the complete UDI.
- For MDSW not delivered on a physical medium but having a user interface (e.g. mobile apps, webtools), only the human-readable interpretation (HRI) of the UDI shall be required. It shall be provided on a readily accessible screen for the user in an easily-readable plain-text format.
- For MDSW lacking a user interface (e.g. middleware for image conversion), the human-readable representation of the UDI shall be conveyed through an application programming interface (API).
- Maintain UDIs throughout the MDSW lifecycle.
Any medical devices and in vitro diagnostic medical devices placed on the market under Regulation (EU) 2017/745 (MDR) or Regulation 2017/746 (IVDR) must have been assigned a Basic UDI-DI and UDI-DI registered in the ‘UDI/Device module’ (UDI database) of EUDAMED.
The obligation to register UDI and devices in EUDAMED will apply 24 months after the Commission publishes a notice the system has achieved full functionality.
Legacy devices are not subject to UDI obligations.
Still, it should be remarked that legacy devices are in fact required to be registered in the EUDAMED database, where UDI registration is conceived. Therefore, for the sake of the workability of EUDAMED, legacy devices registered in EUDAMED will need to have two other unique access keys (IDs) to replace the Basic UDI-DI and UDI-DI.
Those codes will be assigned by EUDAMED itself (or partially by the manufacturer), and will allow the system to work and keep its design as close as possible to the MDR certified products.
In spite of this, for all those legacy devices aiming to be re-certified under MDR/IVDR, the staggered deadlines of the Regulations transitional provisions will be applied when it comes to UDI placement on the labelling of a legacy device:
- MDR transitional provisions:
- 26 May 2026 for class III custom-made implants.
- 31 December 2027 for class III and class IIb implantable devices (except certain devices for which the MDR provides exemptions).
- 31 December 2028 for other class IIb devices and class IIa, class Im, class Is and self-certified class I devices.
- IVDR transitional provisions:
- 26 May 2025 for class D and IVDs with Notified Body issued IVDD CE Marking certificates.
- 26 May 2026 for Class C IVDs.
- 26 May 2027 for Class B IVDs.
- 26 May 2027 for Class A sterile IVDs.
- 26 May 2028 for IVDs used in health institutions.
The general requirements regarding assigning UDI codes to de Medical and In Vitro Diagnostic Devices are similar among international markets. Only the submission deadlines may change. Moreover, the same issuing entities would be the ones in charge of assisting the manufacturers to obtain UDI codes.
